The fight against colorectal cancer is constantly evolving, and one of the most promising areas of advancement lies in immunotherapy. Are you curious about the latest breakthroughs and what the future holds? Immunotherapy harnesses the power of the body's own immune system to target and destroy cancer cells, offering a potentially less toxic and more effective approach compared to traditional treatments. Explore the groundbreaking advancements in immunotherapy for colorectal cancer in 2025, offering hope for more targeted and effective treatment options. This field is rapidly changing, and 2025 promises to bring even more exciting developments.
We'll delve into the specific types of immunotherapy being explored for colorectal cancer, including checkpoint inhibitors, CAR T-cell therapy, and cancer vaccines. We will also address how these therapies work, who might benefit from them, and what the potential side effects are. Furthermore, we'll explore the latest research and clinical trials that are shaping the future of immunotherapy for this challenging disease.
The main goal here is to provide a clear and comprehensive overview of the current state of immunotherapy for colorectal cancer and what advancements we can anticipate in 2025. We hope to empower patients, families, and healthcare professionals with the knowledge they need to make informed decisions about treatment options and to stay abreast of the latest developments in this exciting field.
In summary, immunotherapy is becoming an increasingly important tool in the fight against colorectal cancer. As we move closer to 2025, we can expect to see even more innovative and effective immunotherapy approaches emerge, offering new hope for patients with this disease. It is paramount to stay informed about these advancements, as they could significantly impact the future of colorectal cancer treatment.
Understanding Immunotherapy: A Primer
Immunotherapy isn't a single treatment; it's a whole category of treatments. Think of it like this: your immune system is your body's army, constantly on the lookout for invaders. Cancer cells, however, are sneaky. They can sometimes evade detection or even suppress the immune system's response. Immunotherapy aims to boost the immune system, helping it recognize and destroy cancer cells. It's like giving your army better weapons and training to fight a specific enemy. But how does it actually work? Let's break it down a bit further.
The Different Types of Immunotherapy
There are several different types of immunotherapy currently being used or being researched for colorectal cancer. Each type works in a slightly different way, but the overall goal is the same: to empower the immune system to fight the cancer.
Checkpoint Inhibitors: These are probably the most well-known type of immunotherapy. Imagine checkpoints as brakes on the immune system, preventing it from attacking healthy cells. Cancer cells can sometimes exploit these checkpoints to hide from the immune system. Checkpoint inhibitors release those brakes, allowing the immune system to attack the cancer cells more effectively. Examples include drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo). The thrill of potentially unleashing your immune system’s full power is pretty amazing. CAR T-Cell Therapy: This is a more personalized approach. T-cells, a type of immune cell, are extracted from the patient's blood. In a lab, these T-cells are genetically engineered to express a special receptor, called a chimeric antigen receptor (CAR), that specifically targets the cancer cells. The modified T-cells are then infused back into the patient's body, where they can hunt down and destroy the cancer. Cancer Vaccines: Unlike traditional vaccines that prevent disease, cancer vaccines are designed to treat existing cancer. They work by stimulating the immune system to recognize and attack cancer cells. These vaccines often contain cancer-specific antigens (proteins or other molecules) that trigger an immune response.
Who Benefits from Immunotherapy?
Immunotherapy isn't a one-size-fits-all treatment. It doesn't work for everyone with colorectal cancer. One of the key factors that determines whether someone might benefit from immunotherapy is their microsatellite instability (MSI) status . Cancers with high microsatellite instability (MSI-H) or deficient mismatch repair (dMMR) are more likely to respond to checkpoint inhibitors. These cancers have a lot of genetic mutations, which makes them more visible to the immune system. It's like wearing a bright neon sign that says, "I'm cancer!"
However, research is constantly evolving, and scientists are working to identify other biomarkers that can predict which patients are most likely to benefit from immunotherapy. It can be nerve-wracking waiting for test results, but the potential reward of finding a treatment that works is worth it.
Potential Side Effects
Like any medical treatment, immunotherapy can have side effects. Since immunotherapy affects the immune system, side effects can range from mild to severe and can affect various parts of the body.
Common side effects include:
Fatigue Skin rashes Diarrhea Pneumonitis (inflammation of the lungs) Colitis (inflammation of the colon) Hepatitis (inflammation of the liver)
It's crucial to discuss potential side effects with your doctor before starting immunotherapy. They can help you understand the risks and benefits and monitor you closely for any adverse reactions. It's definitely something to be aware of, but don't let it scare you off completely.
What's New in Immunotherapy for Colorectal Cancer in 2025?
The field of immunotherapy is constantly evolving, with new research and clinical trials emerging all the time. So, what can we expect to see in 2025 when it comes to immunotherapy for colorectal cancer?
Advances in Checkpoint Inhibitors
While checkpoint inhibitors have already shown promise in treating MSI-H/dMMR colorectal cancers, researchers are exploring ways to make them more effective and to expand their use to a broader range of patients.
Combination Therapies: One approach is to combine checkpoint inhibitors with other treatments, such as chemotherapy, targeted therapy, or other immunotherapies. This can help to overcome resistance mechanisms and boost the immune response. Novel Checkpoint Inhibitors: Scientists are also developing new checkpoint inhibitors that target different immune checkpoints. This could provide additional options for patients who don't respond to existing checkpoint inhibitors. Personalized Approaches: Researchers are working to identify biomarkers that can predict which patients are most likely to benefit from specific checkpoint inhibitors. This would allow for a more personalized approach to treatment. The hope is that we’ll see better prediction models and less trial and error.
CAR T-Cell Therapy for Colorectal Cancer
CAR T-cell therapy has shown remarkable success in treating certain blood cancers, but it has been more challenging to develop effective CAR T-cell therapies for solid tumors like colorectal cancer. However, there has been significant progress in this area.
Targeting New Antigens: Researchers are identifying new antigens that are specifically expressed on colorectal cancer cells. This allows them to design CAR T-cells that can more effectively target and destroy the cancer. Overcoming the Tumor Microenvironment: Solid tumors have a complex microenvironment that can suppress the immune system and prevent CAR T-cells from reaching the cancer cells. Scientists are developing strategies to overcome this obstacle, such as modifying the CAR T-cells to make them more resistant to the immunosuppressive effects of the tumor microenvironment. Improving Safety: CAR T-cell therapy can have serious side effects, such as cytokine release syndrome (CRS) and neurotoxicity. Researchers are working to improve the safety of CAR T-cell therapy by developing strategies to control these side effects.
Cancer Vaccines: A Renewed Focus
Cancer vaccines have been around for a while, but they haven't yet achieved the same level of success as checkpoint inhibitors or CAR T-cell therapy. However, there is a renewed focus on cancer vaccines, with researchers exploring new approaches to make them more effective.
Personalized Vaccines: One promising approach is to develop personalized cancer vaccines that are tailored to the specific mutations in a patient's cancer cells. These vaccines can stimulate a more targeted immune response against the cancer. Neoantigen Vaccines: Neoantigens are new antigens that are created as a result of mutations in cancer cells. These antigens are not normally found in the body, so they are more likely to trigger a strong immune response. Combination Strategies: Researchers are also exploring ways to combine cancer vaccines with other immunotherapies, such as checkpoint inhibitors, to boost the immune response.
The Role of the Microbiome
The gut microbiome, the community of microorganisms that live in our intestines, is increasingly recognized as playing a crucial role in cancer development and treatment. Studies have shown that the microbiome can influence the response to immunotherapy.
Modulating the Microbiome: Researchers are investigating ways to modulate the microbiome to improve the efficacy of immunotherapy. This could involve using probiotics, prebiotics, or fecal microbiota transplantation (FMT) to alter the composition of the microbiome. Identifying Predictive Biomarkers: Scientists are also working to identify specific microbial signatures that can predict which patients are most likely to respond to immunotherapy. This could help to personalize treatment decisions.
The Patient Experience: What to Expect
Undergoing immunotherapy can be a complex and emotional experience. It's important to be prepared for what to expect and to have a strong support system in place.
Talking to Your Doctor
The first step is to have an open and honest conversation with your doctor about whether immunotherapy is right for you. Ask questions about the potential benefits and risks, the different types of immunotherapy available, and what to expect during treatment. Don't be afraid to ask for clarification if you don't understand something. It's your body, and you have the right to be fully informed.
Preparing for Treatment
Before starting immunotherapy, your doctor will perform a thorough evaluation to assess your overall health and to determine if you are a good candidate for treatment. You may need to undergo blood tests, imaging scans, and other procedures.
It's also important to prepare yourself mentally and emotionally for treatment. Immunotherapy can be a long and challenging process, so it's important to have realistic expectations and to focus on staying positive.
During Treatment
Immunotherapy is typically administered intravenously, meaning that the drug is injected into a vein. The frequency and duration of treatment will vary depending on the type of immunotherapy being used and the individual patient's response.
During treatment, you will be closely monitored for side effects. It's important to report any unusual symptoms to your doctor immediately.
After Treatment
After completing immunotherapy, you will continue to be monitored for recurrence of cancer. It's important to follow your doctor's recommendations for follow-up care, which may include regular checkups, imaging scans, and blood tests.
FAQ: Immunotherapy for Colorectal Cancer: What’s New in 2025
Let's tackle some of the most frequently asked questions about immunotherapy for colorectal cancer , especially with an eye toward what's new in 2025. It can be a complex topic, so we want to make sure you have the clearest information possible.
General Questions about Immunotherapy
Q: What exactly is immunotherapy?
A: Simply put, immunotherapy is a type of cancer treatment that helps your own immune system fight the cancer. It doesn't directly attack the cancer cells, but instead it empowers your body's natural defenses to do the job. Think of it as giving your immune system a boost or a set of better tools.
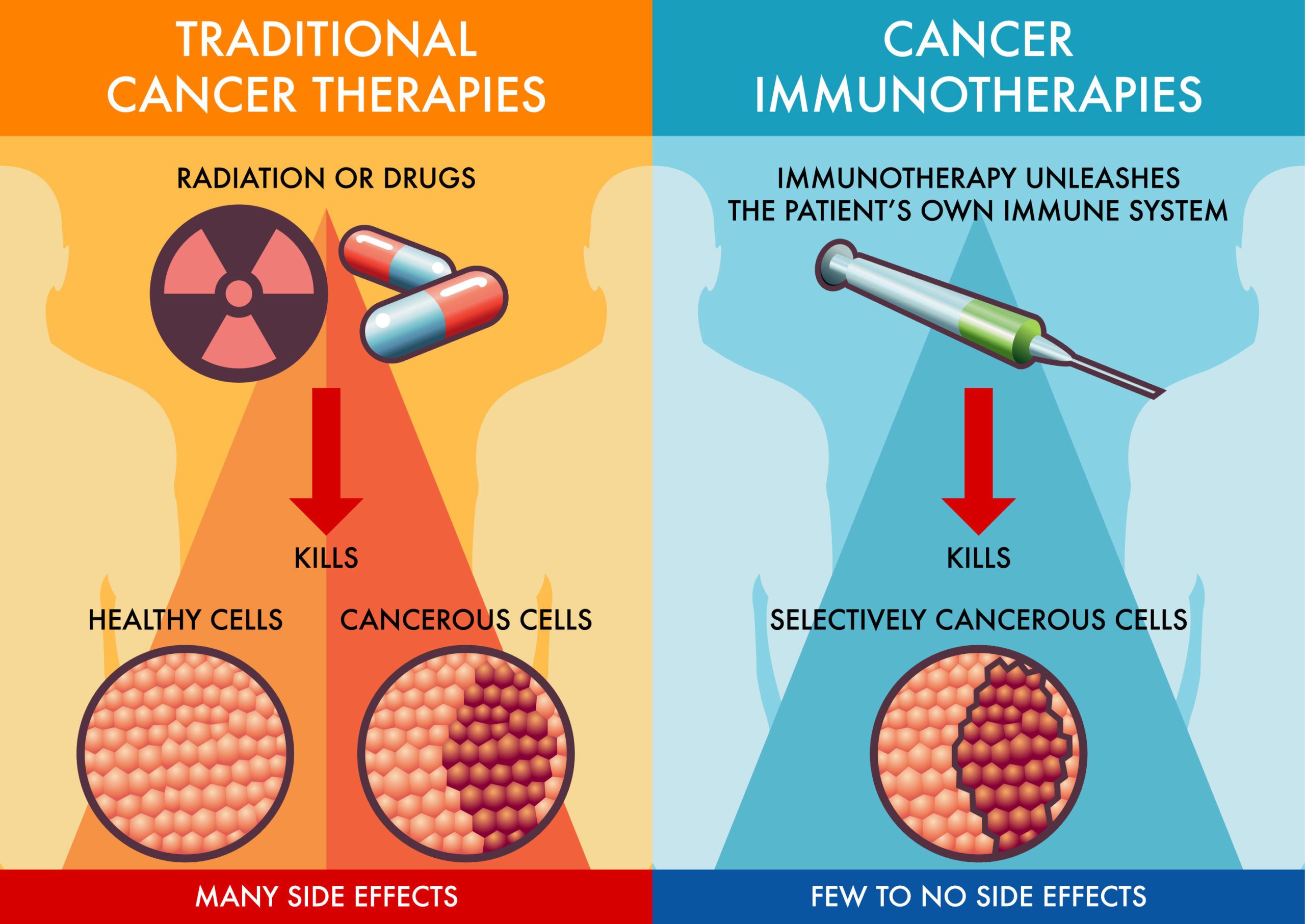
Q: How is immunotherapy different from chemotherapy or radiation?
A: Chemotherapy and radiation therapy directly target and kill cancer cells. However, they can also damage healthy cells, leading to side effects. Immunotherapy, on the other hand, is designed to be more targeted, focusing specifically on the immune system and minimizing damage to healthy tissues. This can result in fewer and less severe side effects for some patients.
Q: Is immunotherapy a cure for colorectal cancer?
A: While immunotherapy has shown remarkable success in some patients with colorectal cancer, it's not a cure for everyone. The effectiveness of immunotherapy depends on several factors, including the type of cancer, the stage of the disease, and the individual patient's immune system. However, for those who respond well, immunotherapy can lead to long-term remission and even a potential cure.
Questions About Specific Types of Immunotherapy
Q: What are checkpoint inhibitors and how do they work?
A: Checkpoint inhibitors are drugs that block certain proteins on immune cells that prevent them from attacking cancer cells. These proteins, called checkpoints, act like brakes on the immune system. By blocking these checkpoints, checkpoint inhibitors release the brakes and allow the immune system to attack the cancer cells more effectively.
Q: What is CAR T-cell therapy and is it used for colorectal cancer?
A: CAR T-cell therapy is a type of immunotherapy in which T cells (a type of immune cell) are taken from a patient's blood, genetically engineered to express a special receptor (CAR) that targets the patient's cancer cells, and then infused back into the patient. While CAR T-cell therapy has been highly successful in treating certain blood cancers, its use in solid tumors like colorectal cancer is still under investigation. However, there has been significant progress in developing CAR T-cell therapies for colorectal cancer.
Q: What are cancer vaccines and how are they different from regular vaccines?
A: Cancer vaccines are designed to treat existing cancer, not to prevent it like traditional vaccines. They work by stimulating the immune system to recognize and attack cancer cells. Cancer vaccines often contain cancer-specific antigens (proteins or other molecules) that trigger an immune response.
Questions About What's New in 2025
Q: What are the most exciting advancements in immunotherapy for colorectal cancer that we can expect to see in 2025?
A: In 2025, we can anticipate several exciting advancements in immunotherapy for colorectal cancer . These include more effective combination therapies using checkpoint inhibitors, progress in developing CAR T-cell therapies that can overcome the challenges of solid tumors, personalized cancer vaccines tailored to individual patients' cancer mutations, and a better understanding of how the gut microbiome influences the response to immunotherapy.
Q: How will these advancements impact patient care?
A: These advancements have the potential to significantly improve patient care by offering more targeted and effective treatment options, reducing side effects, and improving long-term outcomes. Personalized approaches, such as personalized cancer vaccines and microbiome modulation, will allow for more tailored treatment plans based on individual patient characteristics.
Q: Where can I find more information about clinical trials for immunotherapy for colorectal cancer?
A: You can find information about clinical trials for immunotherapy for colorectal cancer on websites such as the National Cancer Institute (NCI), the American Cancer Society (ACS), and ClinicalTrials.gov. Your doctor can also provide you with information about clinical trials that may be a good fit for you.
Questions About Side Effects and Management
Q: What are the common side effects of immunotherapy?
A: Common side effects of immunotherapy can include fatigue, skin rashes, diarrhea, pneumonitis (inflammation of the lungs), colitis (inflammation of the colon), and hepatitis (inflammation of the liver). It's important to note that not everyone experiences these side effects, and the severity can vary.
Q: How are side effects of immunotherapy managed?
A: Side effects of immunotherapy are typically managed with supportive care, such as medications to relieve symptoms, and in some cases, immunosuppressants to dampen the immune response. It's crucial to report any unusual symptoms to your doctor immediately so that they can be managed promptly and effectively.
Q: Will immunotherapy affect my quality of life?
A: Immunotherapy can affect quality of life, depending on the severity of side effects. However, many patients are able to maintain a good quality of life during treatment. Your doctor can help you manage side effects and provide support to help you cope with any challenges you may face. Remember, communication is key!
Moving Forward: The Future of Immunotherapy
The future of immunotherapy for colorectal cancer is bright. With ongoing research and clinical trials, we can expect to see even more innovative and effective approaches emerge in the years to come. It's essential to stay informed about these advancements and to discuss them with your doctor. Immunotherapy might not be a magic bullet, but it's a powerful tool that is changing the landscape of cancer treatment.
While there is still much to learn, the progress that has been made in recent years is truly remarkable. Immunotherapy for colorectal cancer: What’s new in 2025 represents a significant step forward in the fight against this disease, offering new hope for patients and their families. By continuing to invest in research and development, we can unlock the full potential of immunotherapy and improve the lives of countless individuals affected by colorectal cancer. Stay positive, stay informed, and never give up hope.
.png)