Imagine forgetting faces, struggling to find the right words, or feeling increasingly confused. For many individuals battling Parkinson's disease, these cognitive challenges can unfortunately evolve into Parkinson's Disease Dementia: Symptoms, Diagnosis, and Care . Understanding the progression of Parkinson's and its potential impact on cognitive function is vital for patients, caregivers, and healthcare professionals. This decline isn't just about memory lapses; it's a complex condition impacting daily life, requiring specialized attention and tailored support. Explore Parkinson's Disease Dementia: Symptoms, Diagnosis, and Care. Learn about early signs, diagnostic methods, and effective care strategies for improved patient outcomes.
Navigating the complexities of Parkinson's can be daunting, especially when cognitive impairment enters the picture. This article aims to shed light on the various facets of Parkinson's Disease Dementia. We'll delve into recognizing the subtle symptoms , understanding the diagnostic journey, and exploring the available care options that can significantly improve the quality of life for those affected. Gaining a comprehensive understanding of this condition empowers both patients and their support networks to make informed decisions and seek timely intervention.
If you suspect that you or a loved one may be experiencing cognitive changes alongside Parkinson's symptoms, knowing what to look for and how to approach diagnosis and care becomes paramount. We'll cover the key symptoms that differentiate Parkinson's Disease Dementia from typical age-related memory loss, discuss the diagnostic tools and processes used by medical professionals, and explore the range of treatment and support options that can help manage the condition and improve overall well-being.
Ultimately, our goal is to provide a comprehensive resource that empowers you to understand Parkinson's Disease Dementia: Symptoms, Diagnosis, and Care . By equipping you with knowledge about the early symptoms, the diagnostic procedures, and the available care strategies, we hope to enable you to navigate this challenging journey with greater confidence and ensure the best possible quality of life for those affected by this condition.
Understanding Parkinson's Disease Dementia
Parkinson's Disease Dementia (PDD) is a neurodegenerative disorder that can develop in individuals with Parkinson's disease. It's characterized by a progressive decline in cognitive abilities, impacting memory, attention, and executive function. But what exactly sets PDD apart from other forms of dementia and why is it so important to understand its specific characteristics?
What is Parkinson's Disease Dementia?
Unlike Alzheimer's disease, which primarily affects memory in its early stages, PDD often manifests with a broader range of cognitive and behavioral symptoms. These can include difficulties with:
Attention and concentration: Trouble focusing, easily distracted. Executive function: Problems with planning, decision-making, and problem-solving. Visual-spatial skills: Difficulty judging distances, navigating familiar routes, or perceiving spatial relationships. Memory: Forgetfulness, particularly for recent events. Language: Word-finding difficulties, trouble understanding complex instructions. Behavioral changes: Depression, anxiety, irritability, hallucinations, and delusions.
It’s important to note that not everyone with Parkinson's disease will develop dementia, and the onset and severity of cognitive decline can vary greatly from person to person.
How is Parkinson's Disease Related to Dementia?
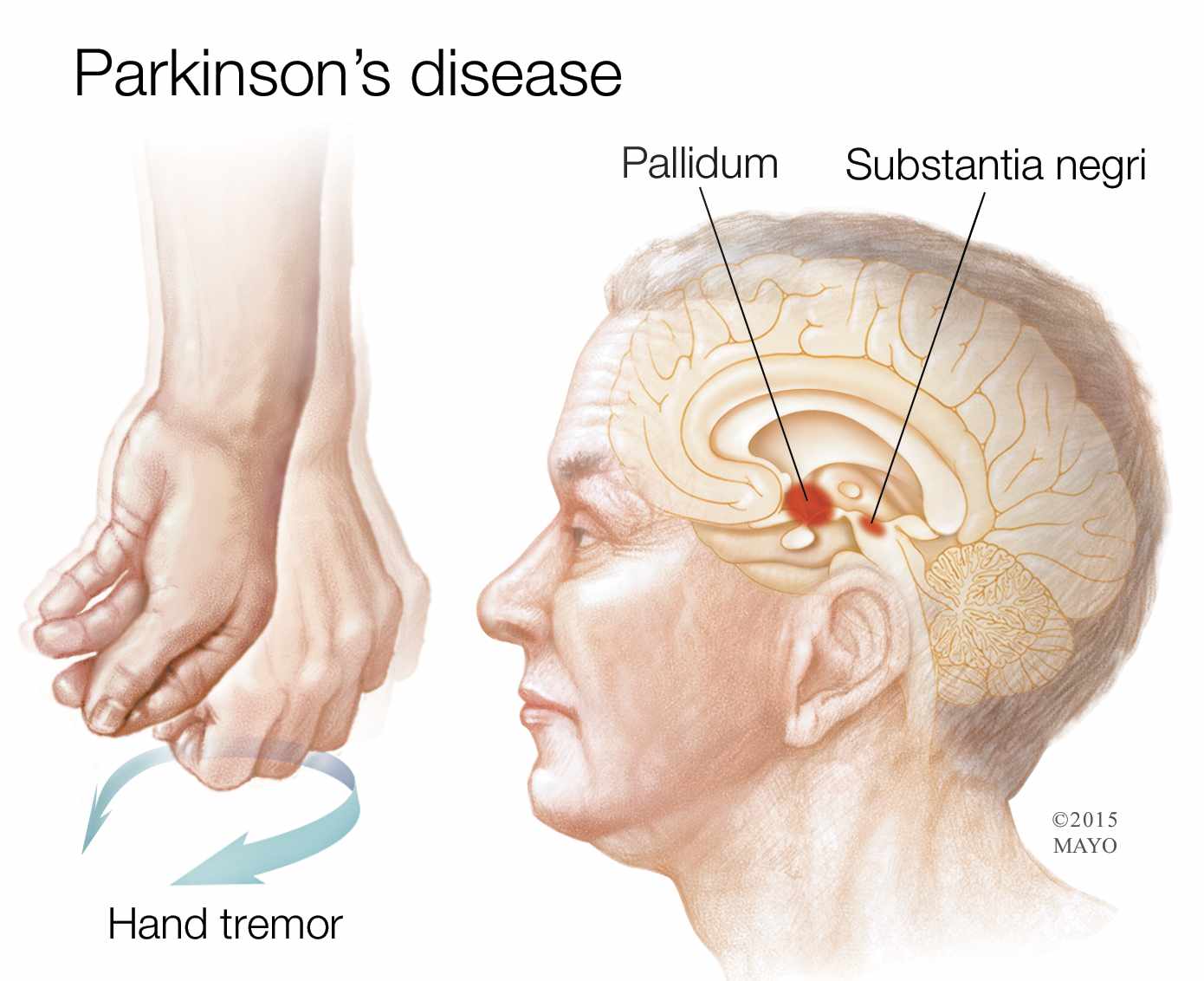
Parkinson's disease primarily affects motor control, causing tremors, rigidity, slow movement, and postural instability. These motor symptoms are caused by the loss of dopamine-producing neurons in a specific area of the brain called the substantia nigra. However, Parkinson's also involves other brain regions and neurotransmitter systems, and these changes can contribute to cognitive decline.
The exact mechanisms underlying PDD are still being researched, but it's believed that the accumulation of Lewy bodies (abnormal protein deposits) in the brain plays a significant role. These Lewy bodies disrupt the normal function of brain cells, leading to both motor and cognitive impairments. Think of it like a computer with damaged circuits – the system might still run, but its performance is significantly degraded.
The Importance of Early Recognition
Early recognition of PDD is crucial for several reasons:
Accurate Diagnosis: Differentiating PDD from other forms of dementia, like Alzheimer's disease or dementia with Lewy bodies (DLB), allows for more targeted treatment and management strategies. Improved Management: Early intervention with medications and therapies can help manage symptoms and improve quality of life. Caregiver Support: Recognizing the challenges associated with PDD allows caregivers to access appropriate support and resources. Planning for the Future: Early diagnosis allows individuals and their families to plan for future care needs and make informed decisions about their long-term well-being.
Symptoms of Parkinson's Disease Dementia
Recognizing the signs of PDD can be challenging, as the symptoms can be subtle and overlap with other conditions. It’s important to remember that not everyone with Parkinson's will develop all of these symptoms , and the severity can vary widely. However, being aware of these potential changes can help you identify them early and seek appropriate medical evaluation.
Cognitive Symptoms
These are the core symptoms related to thinking and mental processes:
Memory Problems: Difficulty remembering recent events, repeating questions, misplacing items. It's not just occasional forgetfulness; it's a persistent and noticeable decline in memory function. Executive Dysfunction: Trouble planning, organizing, and making decisions. Difficulty following instructions, managing finances, or completing complex tasks. Imagine trying to bake a cake without being able to follow the recipe – that’s similar to the challenges faced by someone with executive dysfunction. Attention Deficits: Difficulty focusing, easily distracted, trouble concentrating on tasks. It becomes hard to filter out distractions and maintain focus on the task at hand. Visuospatial Difficulties: Problems with spatial orientation, judging distances, and perceiving visual information. This can manifest as difficulty driving, navigating familiar routes, or understanding maps.
Behavioral and Psychological Symptoms
These symptoms affect mood, behavior, and perception:
Depression: Persistent feelings of sadness, hopelessness, and loss of interest in activities. Anxiety: Excessive worry, nervousness, and fear. Hallucinations: Seeing or hearing things that are not there. These are usually visual hallucinations, often of people or animals. Delusions: False beliefs that are not based on reality. For example, believing that someone is trying to harm them or that they are being watched. Apathy: Lack of motivation, interest, and initiative. A person with apathy may seem indifferent to their surroundings and have little desire to engage in activities. Irritability and Agitation: Feeling easily frustrated, angry, or restless.
Motor Symptoms
While motor symptoms are the hallmark of Parkinson's disease, they can also be affected by dementia:
Worsening Tremors: Increase in the severity or frequency of tremors. Increased Rigidity: Stiffness and resistance to movement. Slower Movement (Bradykinesia): Significant slowing down of movements. Balance Problems: Increased risk of falls due to impaired balance and coordination.
Distinguishing PDD from Other Conditions
It's important to differentiate PDD from other conditions that can cause similar symptoms, such as:
Alzheimer's Disease: Primarily affects memory in its early stages. Dementia with Lewy Bodies (DLB): Shares some similarities with PDD, but hallucinations and fluctuations in cognitive function are more prominent in DLB. Vascular Dementia: Caused by reduced blood flow to the brain, often resulting from strokes. Depression: Can cause cognitive symptoms that mimic dementia. Medication Side Effects: Some medications can cause cognitive impairment.
Diagnosing Parkinson's Disease Dementia
The diagnosis of PDD is a complex process that involves a comprehensive evaluation by a team of healthcare professionals. There isn't a single test that can definitively diagnose PDD; instead, the diagnosis is based on a combination of factors, including medical history, neurological examination, cognitive testing, and sometimes brain imaging.
Diagnostic Process
The diagnostic process typically involves the following steps:
Medical History: The doctor will ask about the patient's medical history, including any existing medical conditions, medications, and family history of dementia or Parkinson's disease. They'll also inquire about the onset and progression of cognitive and motor symptoms. Neurological Examination: This examination assesses motor skills, balance, coordination, reflexes, and sensory function. The doctor will look for signs of Parkinson's disease, such as tremors, rigidity, and slow movement. Cognitive Testing: This involves a series of tests to evaluate different aspects of cognitive function, including memory, attention, language, executive function, and visuospatial skills. Common tests include the Mini-Mental State Examination (MMSE), the Montreal Cognitive Assessment (MoCA), and neuropsychological testing. Psychiatric Evaluation: A mental health professional may assess the patient for depression, anxiety, hallucinations, delusions, and other behavioral or psychological symptoms. Brain Imaging: MRI or CT scans may be used to rule out other causes of cognitive decline, such as strokes, tumors, or hydrocephalus. Sometimes, a DaTscan (dopamine transporter scan) may be used to help confirm the diagnosis of Parkinson's disease. Review of Medications: The doctor will review the patient's medications to identify any drugs that could be contributing to cognitive impairment.
Diagnostic Criteria
The Movement Disorder Society (MDS) has established diagnostic criteria for PDD, which include:
Established Diagnosis of Parkinson's Disease: The patient must have a prior diagnosis of Parkinson's disease, based on established clinical criteria. Dementia: The patient must meet criteria for dementia, which is defined as a significant decline in cognitive function that interferes with daily activities. Onset of Dementia: The dementia must develop at least one year after the onset of motor symptoms of Parkinson's disease. This helps to differentiate PDD from dementia with Lewy bodies (DLB), in which cognitive symptoms typically occur before or concurrently with motor symptoms.
Challenges in Diagnosis
Diagnosing PDD can be challenging for several reasons:
Overlapping Symptoms: The symptoms of PDD can overlap with other conditions, such as Alzheimer's disease, dementia with Lewy bodies, and depression. Variability in Symptoms: The symptoms of PDD can vary significantly from person to person, making it difficult to establish a clear diagnosis. Lack of Biomarkers: There are currently no specific biomarkers for PDD, making it difficult to confirm the diagnosis with laboratory tests. Subjectivity of Cognitive Testing: Cognitive testing relies on the patient's performance, which can be influenced by factors such as motivation, fatigue, and anxiety.
The Importance of a Multidisciplinary Approach
Given the complexities of diagnosing PDD, a multidisciplinary approach is essential. This involves collaboration among neurologists, psychiatrists, neuropsychologists, and other healthcare professionals to ensure a comprehensive evaluation and accurate diagnosis.
Care and Management of Parkinson's Disease Dementia
While there is no cure for PDD, there are various strategies to manage symptoms, improve quality of life, and provide support for both patients and caregivers. The approach to care is often multidisciplinary, involving medications, therapies, lifestyle modifications, and supportive services.
Medications
Several medications can be used to manage the symptoms of PDD:
Cholinesterase Inhibitors: These medications, such as donepezil, rivastigmine, and galantamine, can help improve cognitive function by increasing the levels of acetylcholine, a neurotransmitter that is important for memory and learning. These are often used to treat Alzheimer's disease as well. Memantine: This medication, an NMDA receptor antagonist, can also improve cognitive function, particularly in individuals with moderate to severe PDD. Antidepressants: Selective serotonin reuptake inhibitors (SSRIs) are often used to treat depression and anxiety, which are common in PDD. Antipsychotics: These medications may be used to manage hallucinations, delusions, and agitation, but they should be used with caution due to potential side effects. Always discuss the risks and benefits with a doctor.
Therapies
Various therapies can help manage the symptoms of PDD and improve quality of life:
Cognitive Rehabilitation: This therapy aims to improve cognitive function through targeted exercises and strategies. It can help individuals with PDD improve their memory, attention, and problem-solving skills. Speech Therapy: Speech therapy can help individuals with PDD improve their communication skills, including speech, language, and swallowing. Occupational Therapy: Occupational therapy can help individuals with PDD maintain their independence and perform daily activities more easily. This may involve adapting the environment, using assistive devices, and learning new strategies for completing tasks. Physical Therapy: Physical therapy can help individuals with PDD improve their motor skills, balance, and coordination. This can reduce the risk of falls and improve overall mobility. Psychotherapy: Psychotherapy, such as cognitive-behavioral therapy (CBT), can help individuals with PDD manage depression, anxiety, and other emotional challenges.
Lifestyle Modifications
Several lifestyle modifications can help manage the symptoms of PDD:
Regular Exercise: Regular physical activity can improve motor function, cognitive function, and mood. Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains can promote brain health and overall well-being. Cognitive Stimulation: Engaging in mentally stimulating activities, such as reading, puzzles, and games, can help maintain cognitive function. Social Engagement: Maintaining social connections and engaging in social activities can help reduce feelings of isolation and depression. Adequate Sleep: Getting enough sleep is essential for cognitive function and overall health.
Caregiver Support
Caregivers play a vital role in the care of individuals with PDD. Providing support to caregivers is essential for their well-being and their ability to provide quality care.
Education and Training: Caregivers need education and training on PDD, its symptoms, and how to manage them. Support Groups: Support groups provide a forum for caregivers to share their experiences, learn from others, and receive emotional support. Respite Care: Respite care provides temporary relief for caregivers, allowing them to take a break and recharge. Counseling: Counseling can help caregivers cope with the stress and emotional challenges of caring for someone with PDD.
Creating a Supportive Environment
Creating a safe and supportive environment can help individuals with PDD maintain their independence and quality of life:
Simplify the Environment: Reduce clutter and distractions to make it easier for the individual to navigate their surroundings. Provide Clear and Simple Instructions: Use clear and simple language when communicating with the individual. Establish a Routine: Maintaining a consistent routine can help reduce confusion and anxiety. Use Visual Aids: Use visual aids, such as pictures and labels, to help the individual remember important information and perform tasks. Ensure Safety: Take steps to ensure the individual's safety, such as removing hazards and installing grab bars in the bathroom.
Frequently Asked Questions (FAQ)
What are the early signs of Parkinson's Disease Dementia?
Early signs of Parkinson's Disease Dementia: Symptoms, Diagnosis, and Care include subtle changes in cognitive function, such as difficulty with attention, planning, and problem-solving. Memory problems may also be present, but they are often less prominent than in Alzheimer's disease. Behavioral changes, such as depression, anxiety, and apathy, can also be early indicators.
How is PDD different from Alzheimer's disease?
While both PDD and Alzheimer's disease are forms of dementia, they differ in several key aspects. Alzheimer's disease primarily affects memory in its early stages, while PDD often presents with a broader range of cognitive and behavioral symptoms. In PDD, motor symptoms of Parkinson's disease typically precede the onset of cognitive decline, whereas in Alzheimer's disease, memory loss is usually the first noticeable symptom.
Is there a cure for Parkinson's Disease Dementia?
Unfortunately, there is currently no cure for PDD. However, various treatments and therapies can help manage the symptoms and improve quality of life. These include medications, cognitive rehabilitation, speech therapy, occupational therapy, physical therapy, and psychotherapy.
What can I do to help a loved one with PDD?
Supporting a loved one with PDD requires patience, understanding, and a proactive approach.
How can caregivers manage the challenges of PDD?
Caregivers can manage the challenges of PDD by educating themselves about the condition, seeking support from support groups and other resources, taking breaks to avoid burnout, and creating a safe and supportive environment for their loved one. Effective communication strategies, such as using clear and simple language, can also be helpful.
Are there any lifestyle changes that can help manage PDD symptoms?
Yes, several lifestyle changes can help manage PDD symptoms. These include regular exercise, a healthy diet, cognitive stimulation, social engagement, and adequate sleep. These lifestyle modifications can improve motor function, cognitive function, mood, and overall well-being.
What resources are available for individuals with PDD and their families?
Numerous resources are available for individuals with PDD and their families.
Where can I find support groups for PDD caregivers?
Support groups for PDD caregivers can be found through organizations such as the Parkinson's Foundation, the Lewy Body Dementia Association (LBDA), and local hospitals and clinics. Online support groups are also available.
What financial assistance programs are available for individuals with PDD?
Financial assistance programs for individuals with PDD may include Social Security Disability Insurance (SSDI), Supplemental Security Income (SSI), Medicaid, and Veterans Affairs (VA) benefits. Eligibility requirements vary depending on the program.
Conclusion
Understanding Parkinson's Disease Dementia: Symptoms, Diagnosis, and Care is crucial for individuals affected, their families, and healthcare professionals. While the diagnosis can be challenging, recognizing the early symptoms, seeking timely medical evaluation, and implementing appropriate care strategies can significantly improve quality of life. A multidisciplinary approach, involving medications, therapies, lifestyle modifications, and caregiver support, is essential for managing the complex challenges associated with PDD. By raising awareness and providing comprehensive resources, we can empower those affected by PDD to live as fulfilling lives as possible.
.png)