Parkinson’s Disease is a progressive neurological disorder that impacts movement. Imagine a life where simple tasks like buttoning a shirt or pouring a cup of coffee become monumental challenges. This is the reality for many living with Parkinson's. Recognizing the early signs and symptoms is crucial for timely diagnosis and management, potentially slowing its progression and improving quality of life. What if you could identify the subtle clues that could make all the difference? This article will explore what Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore are and empower you to take proactive steps.
Understanding Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore involves more than just recognizing the obvious tremors. It's about being aware of subtle changes in motor skills, non-motor symptoms, and overall well-being. The importance of early detection lies in the potential to implement interventions, such as medication, physical therapy, and lifestyle adjustments, that can significantly impact the disease's trajectory. Ignoring these early warning signs can lead to delayed diagnosis and missed opportunities for optimizing treatment.
Why should you care about Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore ? Because knowledge is power. Being informed allows you to advocate for yourself or loved ones, seek timely medical attention, and make informed decisions about treatment options. Early diagnosis provides access to resources and support groups that can help manage the physical, emotional, and social challenges associated with Parkinson's. It's about empowering yourself to take control and live the best possible life despite the diagnosis.
This exploration into Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore will arm you with the information needed to recognize potential red flags. By understanding the nuanced ways in which Parkinson's can manifest, you'll be better equipped to seek medical advice and embark on a path of proactive management. Remember, early detection is key to maximizing quality of life and slowing the disease's progression. Now, let's delve into the specifics and uncover what you need to know.
Understanding Parkinson's Disease
Parkinson's Disease is a neurodegenerative disorder that primarily affects dopamine-producing neurons in the brain. Dopamine is a neurotransmitter that plays a crucial role in controlling movement, coordination, and balance. When these neurons are damaged or die, the brain produces less dopamine, leading to the characteristic motor symptoms of Parkinson's.
The exact cause of Parkinson's Disease is not fully understood, but it is believed to be a combination of genetic and environmental factors. While some cases are linked to specific gene mutations, most are sporadic, meaning they occur without a clear family history. Risk factors include age, exposure to certain toxins, and a family history of Parkinson's.
Parkinson's Disease is a progressive disorder, meaning that its symptoms worsen over time. The rate of progression varies from person to person, but the disease can eventually lead to significant disability. However, with proper management and treatment, people with Parkinson's can live active and fulfilling lives for many years.
A Brief History of Parkinson's Disease
Parkinson's Disease was first described in detail by Dr. James Parkinson in his 1817 essay, "An Essay on the Shaking Palsy." In this essay, he outlined the key symptoms of the disease, including tremor, rigidity, and postural instability.
Over the years, researchers have made significant progress in understanding the underlying mechanisms of Parkinson's Disease and developing treatments to manage its symptoms. The discovery of dopamine's role in Parkinson's Disease in the 1960s led to the development of levodopa, a medication that remains the gold standard for treating motor symptoms.
Despite these advances, there is still no cure for Parkinson's Disease. However, ongoing research is focused on developing new therapies that can slow the progression of the disease and improve the quality of life for those affected.
Early Motor Symptoms of Parkinson's Disease
The motor symptoms of Parkinson's Disease are often the most noticeable and debilitating. These symptoms are caused by the loss of dopamine-producing neurons in the brain and can significantly impact a person's ability to move and function independently.
It's important to remember that not everyone with Parkinson's will experience all of these symptoms, and the severity of symptoms can vary greatly from person to person. Early recognition of these motor symptoms is crucial for timely diagnosis and treatment.
Tremor
Tremor is one of the most well-known symptoms of Parkinson's Disease. It typically starts in one hand or arm and may spread to other parts of the body over time. The tremor is usually a resting tremor , meaning that it occurs when the limb is at rest and disappears or lessens with voluntary movement.
The tremor is often described as a "pill-rolling" tremor because it resembles the motion of rolling a pill between the thumb and forefinger. It can also affect the legs, jaw, or face. While tremor is a hallmark symptom of Parkinson's, it's important to note that not everyone with Parkinson's experiences tremor, and tremor can also be caused by other conditions.
Rigidity
Rigidity is another common motor symptom of Parkinson's Disease. It refers to stiffness or inflexibility of the muscles, which can make it difficult to move and can cause pain. Rigidity can affect any part of the body, but it is most often felt in the limbs, neck, and trunk.
There are two main types of rigidity:
Lead-pipe rigidity: This type of rigidity is characterized by a constant resistance to movement throughout the range of motion. Cogwheel rigidity: This type of rigidity is characterized by a jerky, ratchety feeling when the limb is moved.
Rigidity can make everyday tasks like dressing, bathing, and eating difficult. It can also contribute to fatigue and pain.
Bradykinesia
Bradykinesia refers to slowness of movement and is a core feature of Parkinson's Disease. It can affect a wide range of movements, from simple actions like buttoning a shirt to more complex activities like walking.
Bradykinesia can manifest in several ways, including:
Difficulty initiating movement: It may take longer than usual to start a movement, such as getting out of a chair or starting to walk. Slowed movement: Movements may be performed more slowly and deliberately than usual. Reduced amplitude of movement: Movements may be smaller and less forceful than usual. Fatigue: Bradykinesia can contribute to fatigue, as it requires more effort to perform even simple tasks.
Bradykinesia can significantly impact a person's ability to perform daily activities and can lead to feelings of frustration and helplessness.
Postural Instability
Postural instability refers to impaired balance and coordination, which can increase the risk of falls. It is often a later symptom of Parkinson's Disease, but it can sometimes be present in the early stages.
Postural instability is caused by the loss of dopamine-producing neurons in the brain, which affects the ability to maintain balance and coordination. People with postural instability may have difficulty standing upright, may sway or lean to one side, and may have a tendency to fall.
Postural instability can be a significant safety concern for people with Parkinson's Disease, as it can lead to serious injuries from falls. Physical therapy and assistive devices, such as canes or walkers, can help improve balance and coordination and reduce the risk of falls.
Other Motor Symptoms
In addition to tremor, rigidity, bradykinesia, and postural instability, there are several other motor symptoms that can occur in Parkinson's Disease, including:
Freezing: This refers to a sudden, temporary inability to move, often occurring when starting to walk or turning. Shuffling gait: This is a characteristic walking pattern in which the steps are short and shuffling, and the feet may not be lifted properly. Masked face: This refers to a reduction in facial expression, which can make it difficult to convey emotions. Micrographia: This refers to small, cramped handwriting. Dysarthria: This refers to difficulty speaking clearly. Dysphagia: This refers to difficulty swallowing.
These motor symptoms can significantly impact a person's quality of life and can require a multidisciplinary approach to management.
Early Non-Motor Symptoms of Parkinson's Disease
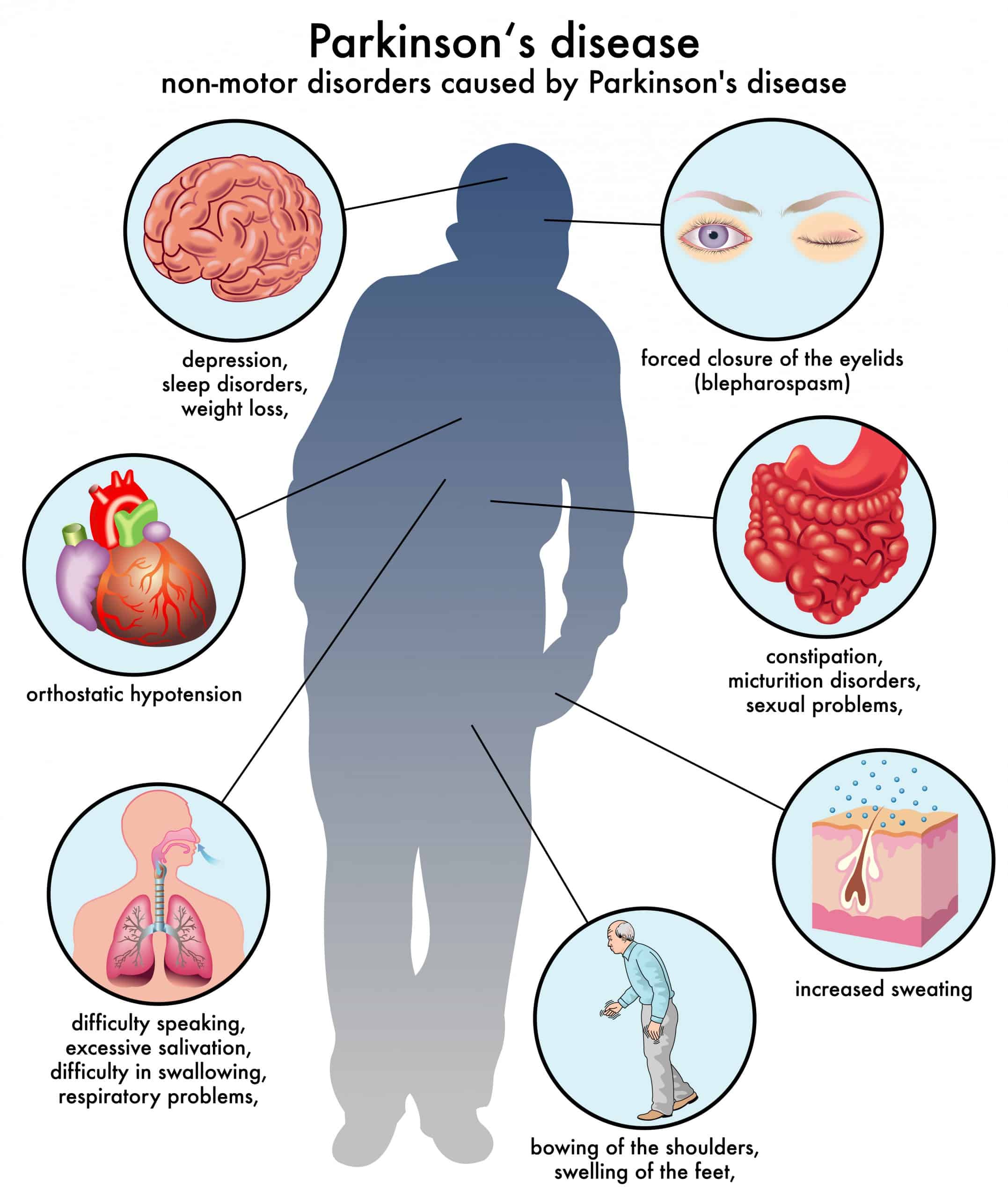
While motor symptoms are the most well-known features of Parkinson's Disease, non-motor symptoms are also common and can significantly impact a person's quality of life. These symptoms can occur even before the onset of motor symptoms and can sometimes be mistaken for other conditions.
It's important to be aware of these non-motor symptoms and to discuss them with a doctor if you experience them, especially if you also have any of the motor symptoms described above.
Loss of Smell (Anosmia)
Loss of smell, also known as anosmia, is one of the earliest and most common non-motor symptoms of Parkinson's Disease. It can occur years before the onset of motor symptoms and is often overlooked or attributed to other causes, such as allergies or a cold.
The loss of smell in Parkinson's Disease is caused by the accumulation of alpha-synuclein protein in the olfactory bulb, which is the part of the brain responsible for processing smells. This accumulation damages the nerve cells in the olfactory bulb, leading to a decreased ability to detect odors.
If you notice a significant decline in your sense of smell, especially if it is accompanied by other potential symptoms of Parkinson's, it's important to see a doctor for evaluation.
Sleep Disturbances
Sleep disturbances are very common in Parkinson's Disease and can take many forms, including:
REM sleep behavior disorder (RBD): This is a condition in which people act out their dreams during REM sleep, which can involve yelling, punching, kicking, or falling out of bed. RBD is a strong predictor of developing Parkinson's Disease or other neurodegenerative disorders. Insomnia: This refers to difficulty falling asleep or staying asleep. Excessive daytime sleepiness: This refers to feeling excessively tired during the day, even after getting enough sleep at night. Restless legs syndrome (RLS): This is a condition in which people experience an uncomfortable sensation in their legs, often accompanied by an urge to move them, which can make it difficult to fall asleep.
Sleep disturbances can significantly impact a person's quality of life and can contribute to fatigue, mood changes, and cognitive problems.
Constipation
Constipation is another common non-motor symptom of Parkinson's Disease. It is often caused by the slowing of movement in the digestive system, which can make it difficult to pass stool.
Constipation can lead to a variety of problems, including abdominal pain, bloating, and nausea. It can also contribute to fatigue and discomfort.
Mood Changes
Mood changes, such as depression and anxiety, are very common in Parkinson's Disease. These mood changes are not simply a reaction to the challenges of living with Parkinson's; they are believed to be caused by changes in brain chemistry related to the disease itself.
Depression can manifest as feelings of sadness, hopelessness, and loss of interest in activities that were once enjoyable. Anxiety can manifest as feelings of worry, nervousness, and fear.
Mood changes can significantly impact a person's quality of life and can make it difficult to cope with the challenges of Parkinson's.
Cognitive Changes
Cognitive changes, such as problems with memory, attention, and executive function, can also occur in Parkinson's Disease. These changes can be subtle in the early stages but can become more pronounced as the disease progresses.
Cognitive changes can affect a person's ability to perform daily tasks, such as managing finances, following instructions, and making decisions. They can also contribute to feelings of frustration and confusion.
Other Non-Motor Symptoms
In addition to the non-motor symptoms described above, there are several other non-motor symptoms that can occur in Parkinson's Disease, including:
Orthostatic hypotension: This refers to a drop in blood pressure upon standing, which can cause dizziness or lightheadedness. Sweating: Some people with Parkinson's Disease experience excessive sweating. Urinary problems: Some people with Parkinson's Disease experience urinary urgency, frequency, or incontinence. Pain: Pain is a common symptom of Parkinson's Disease and can be caused by muscle stiffness, joint problems, or nerve damage. Visual disturbances: Some people with Parkinson's Disease experience visual disturbances, such as blurred vision or double vision.
These non-motor symptoms can significantly impact a person's quality of life and can require a multidisciplinary approach to management.
Diagnosis and Management of Parkinson's Disease
Diagnosing Parkinson's Disease can be challenging, especially in the early stages. There is no single test that can definitively diagnose the disease. Instead, doctors rely on a combination of factors, including a person's medical history, a neurological examination, and response to medication.
The neurological examination typically involves assessing a person's motor skills, such as tremor, rigidity, bradykinesia, and postural instability. The doctor may also assess a person's non-motor symptoms, such as loss of smell, sleep disturbances, and mood changes.
If the doctor suspects Parkinson's Disease, they may order imaging tests, such as a MRI or a DaTscan, to rule out other conditions and to help confirm the diagnosis. A DaTscan is a special type of brain scan that can measure the amount of dopamine transporter in the brain.
Treatment Options
While there is no cure for Parkinson's Disease, there are several treatment options available to manage the symptoms and improve the quality of life for those affected. These treatments include:
Medications: Medications are the mainstay of treatment for Parkinson's Disease. The most common medication is levodopa, which is converted into dopamine in the brain. Other medications include dopamine agonists, MAO-B inhibitors, and COMT inhibitors. Deep brain stimulation (DBS): DBS is a surgical procedure in which electrodes are implanted in the brain to stimulate specific areas involved in motor control. DBS can help reduce tremor, rigidity, and bradykinesia. Physical therapy: Physical therapy can help improve motor skills, balance, and coordination. Occupational therapy: Occupational therapy can help people with Parkinson's Disease adapt to their limitations and maintain their independence. Speech therapy: Speech therapy can help improve speech clarity and swallowing function. Lifestyle modifications: Lifestyle modifications, such as exercise, a healthy diet, and stress management, can also help manage the symptoms of Parkinson's Disease.
The best treatment approach for Parkinson's Disease is individualized and depends on the severity of the symptoms and the person's overall health.
Living with Parkinson's Disease
Living with Parkinson's Disease can be challenging, but there are many things that people with Parkinson's can do to maintain their quality of life. These include:
Staying active: Exercise is important for maintaining motor skills, balance, and coordination. Eating a healthy diet: A healthy diet can help maintain energy levels and prevent constipation. Managing stress: Stress can worsen the symptoms of Parkinson's Disease. Joining a support group: Support groups can provide emotional support and practical advice. Staying connected with friends and family: Social support is important for maintaining emotional well-being. Advocating for yourself: It's important to be an active participant in your own care and to advocate for your needs.
With proper management and support, people with Parkinson's Disease can live active and fulfilling lives.
FAQ: Parkinson's Disease
This section addresses frequently asked questions about Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore . We'll cover everything from genetics to lifestyle changes.
Understanding Parkinson's Disease
Is Parkinson's Disease hereditary?
While genetics can play a role in some cases, most instances of Parkinson's are not directly inherited. However, having a family history of Parkinson's may slightly increase your risk.
What is the average age of onset for Parkinson's Disease?
The average age of onset is around 60, but it can affect people younger than 50 (young-onset Parkinson's).
Are there any environmental factors that increase the risk of Parkinson's Disease?
Exposure to certain pesticides and herbicides has been linked to an increased risk, although more research is needed.
Recognizing Early Signs and Symptoms
Can I have Parkinson's Disease without a tremor?
Yes, absolutely! Tremor is a common symptom, but not everyone with Parkinson's experiences it. Other early signs like rigidity, slow movement, and loss of smell can also be indicative.
What should I do if I suspect I have Parkinson's Disease?
Consult a neurologist. They can perform a thorough examination and order the necessary tests to determine if you have Parkinson's or another condition.
How is Parkinson's Disease diagnosed?
Diagnosis typically involves a neurological exam, review of medical history, and sometimes imaging tests like a DaTscan. There isn't a single definitive test.
Treatment and Management
Can Parkinson's Disease be cured?
Unfortunately, there is currently no cure for Parkinson's Disease, but treatments are available to manage symptoms and improve quality of life.
What are the main types of medications used to treat Parkinson's Disease?
Levodopa, dopamine agonists, MAO-B inhibitors, and COMT inhibitors are commonly prescribed medications.
How can physical therapy help with Parkinson's Disease?
Physical therapy can improve motor skills, balance, and coordination, helping individuals maintain independence and reduce the risk of falls.
Lifestyle and Support
Are there any lifestyle changes that can help manage Parkinson's Disease?
Yes! Regular exercise, a healthy diet, stress management, and adequate sleep can significantly impact symptom management.
Where can I find support groups for Parkinson's Disease?
Organizations like the Parkinson's Foundation and the American Parkinson Disease Association offer resources and support groups for individuals and families affected by Parkinson's.
What role does diet play in managing Parkinson's Disease?
A balanced diet rich in fiber, fruits, and vegetables can help manage constipation and maintain overall health. Staying hydrated is also crucial.
Conclusion: Empowering Yourself with Knowledge
Understanding Parkinson's Disease: Early Signs and Symptoms You Shouldn't Ignore is the first step toward proactive management and a better quality of life. Recognizing the subtle early signs, from loss of smell and sleep disturbances to changes in motor skills, allows for timely diagnosis and intervention. While there's no cure, available treatments and lifestyle modifications can significantly slow the disease's progression and improve daily functioning. By staying informed, seeking medical advice when needed, and connecting with support resources, individuals can empower themselves to live well with Parkinson's. Don't hesitate to prioritize your health and well-being; early detection can make all the difference.
.png)